Metoprolol belongs to a class of drugs called Beta-blockers or beta-adrenergic blockers. Certain functions of body are governed or regulated by the sympathetic nervous system and some are mediated through secretion of adrenaline, acting on the Beta-adrenergic receptors located on target organs; those drugs block these receptors are called as Beta-blockers.
Many functions of heart are regulated through adrenaline. Those may be: increase in heart rate, increase in contractability of heart muscles and increase in oxygen consumption by the muscles.
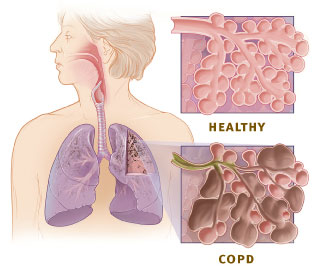
Metoprolol is a cheaper drug with relatively Beta-1-selectivity action i.e. more action over heart; in higher doses, it may also block the Beta-2-receptors located in lungs.
It has been seen that early treatment of myocardial infarction with metoprolol, while in transit to the hospital, can significantly reduce damage to the heart muscles, according to clinical trial study results published Oct. 1 in the journal Circulation.
The study was a collaboration between Centro Nacional de Investigaciones Cardiovasculares Carlos III (CNIC) in Spain and Icahn School of Medicine at Mount Sinai in New York.
Currently, these drugs are mostly not used in emergency treatment of patients for angioplasty in the “door to balloon time” i.e. time taken from arrival in hospital to angioplasty or even before that. This is a critical period to restrict damage to the cardiac muscles to which blood supply can be re-established, called re-perfusion with any of the procedures to remove the blocking agent in the coronary arteries like a thrombus.
In addition to the high risk of death during the infarction, survivors are likely to suffer from heart failure and severe arrhythmias, and often may die in the months or years following the attack. The larger the infarct (death of cardiac muscle), the greater the probability that survivors will suffer these complications in the future.
In other words, the minimum is the damage to the heart muscles in this time, the better is the recovery and final outcome through out the succeeding years to come.
Borja Ibáñez, MD, PhD, head of the Experimental Cardiology Group at CNIC and clinical cardiologist at the Hospital Clínico San Carlos in Spain, is the joint lead investigator of this novel study with Valentín Fuster, MD, PhD, General Director of CNIC, who also serves as Director of Mount Sinai Heart and Physician-in-Chief at The Mount Sinai Medical Center. Also, Dr. Fuster will begin his term in 2014 as the next Editor-in-Chief of the Journal of the American College of Cardiology (JACC).
Metoprolol, a drug of the beta-blocker family, has been available for more than 30 years to treat arterial hypertension and other cardiovascular conditions.
In this new study, the team of researchers were able to examine the potential usefulness of metoprolol after a heart attack. The clinical trial named METOCARD-CNIC is the first to test metoprolol therapy, in heart attack patients undergoing standard angioplasty treatment procedures.
A total of 270 patients with infarction were recruited since 2010 in four of Spain's regions including: Madrid, Galicia, León, and Cantabria. In the randomized study, patients were assigned to receive either intravenous metoprolol or a placebo treatment at the moment of diagnosis of a myocardial infarction during ambulance transit to the catheterization laboratory.
Hospitals in Spain participating in the METOCARD-CNIC trial included: Hospital Clínico San Carlos, Hospital de La Princesa, Hospital 12 de Octubre, Hospital Puerta de Hierro, and Hospital Quirón (Madrid), Hospital Meixoeiro (Galicia), Hospital de León (León), and Hospital Marqués de Valdecilla (Cantabria).
The efficacy of the medical intervention was evaluated by magnetic resonance imaging (MRI) a week after the infarction. MRI measured the mass of damaged heart tissue in all patients. The results showed patients who received metoprolol had much smaller infarcts than those who received the control treatment, and that this smaller infarct size was linked to greater heart contractility.
The MRI scans were analyzed at the central CNIC laboratory by cardiologists blinded to the treatment.
Their preclinical research findings about metoprolol in animal models, analyzed using MRI and published in the journal Circulation in 2007, showed early administration of metoprolol during heart attack increased myocardial salvage.
The molecular mechanism leading to the beneficial effects is not clearly understood. It may have additional route of action, apart from decreasing the heart rate, myocardial contactability and decreasing the oxygen consumption; such as action on platelets and inflammation.
Metoprolol treatment is to be started in a patient, once the clinical parameters like bradycardia (Lower than normal heart rate) and hypotension (Lower than normal Blood pressure) are stabilized and the hemodynamic status had been carefully evaluated for signs of shock and congestive heart failure. Subjects are ineligible for treatment with metoprolol, if hypotension, bradycardia and peripheral shock are present.
Metoprolol to be started in haemodynamically stable patients with the intravenous administration of three bolus injections of 5 mg each at approximately 2 minutes of intervals. During the intravenous administration blood pressure, heart rate, and electrocardiogram are to be monitored.
In patients who tolerate the full intravenous dose (15 mg), Metoprolol tartrate is to be started orally, 50 mg every 6 hours; 15 minutes after the last intravenous dose and be continued for 48 hours. Thereafter, the maintenance dosage is 100 mg twice daily, at least for 3 months; and may be continued for 1 to 3 years according to some researchers.
Patients who appear not to tolerate the full intravenous dose, Metoprolol tartrate tablets may be started, either 25 mg or 50 mg every 6 hours (depending on the degree of intolerance) 15 minutes after the last intravenous dose or as soon as their clinical condition allows. In patients with severe intolerance, Metoprolol tartrate is to be discontinued.
In country like India, metoprolol treatment of myocardial infarction will be beneficial to many, even in the long term considering the cost of follow up treatment of the disease and its' complications; such as heart failure and arrhythmia.
Many functions of heart are regulated through adrenaline. Those may be: increase in heart rate, increase in contractability of heart muscles and increase in oxygen consumption by the muscles.
Metoprolol is a cheaper drug with relatively Beta-1-selectivity action i.e. more action over heart; in higher doses, it may also block the Beta-2-receptors located in lungs.
| Animated sagittal MRI slice of my beating heart (Photo credit: Wikipedia) |
It has been seen that early treatment of myocardial infarction with metoprolol, while in transit to the hospital, can significantly reduce damage to the heart muscles, according to clinical trial study results published Oct. 1 in the journal Circulation.
The study was a collaboration between Centro Nacional de Investigaciones Cardiovasculares Carlos III (CNIC) in Spain and Icahn School of Medicine at Mount Sinai in New York.
Currently, these drugs are mostly not used in emergency treatment of patients for angioplasty in the “door to balloon time” i.e. time taken from arrival in hospital to angioplasty or even before that. This is a critical period to restrict damage to the cardiac muscles to which blood supply can be re-established, called re-perfusion with any of the procedures to remove the blocking agent in the coronary arteries like a thrombus.
In addition to the high risk of death during the infarction, survivors are likely to suffer from heart failure and severe arrhythmias, and often may die in the months or years following the attack. The larger the infarct (death of cardiac muscle), the greater the probability that survivors will suffer these complications in the future.
In other words, the minimum is the damage to the heart muscles in this time, the better is the recovery and final outcome through out the succeeding years to come.
Borja Ibáñez, MD, PhD, head of the Experimental Cardiology Group at CNIC and clinical cardiologist at the Hospital Clínico San Carlos in Spain, is the joint lead investigator of this novel study with Valentín Fuster, MD, PhD, General Director of CNIC, who also serves as Director of Mount Sinai Heart and Physician-in-Chief at The Mount Sinai Medical Center. Also, Dr. Fuster will begin his term in 2014 as the next Editor-in-Chief of the Journal of the American College of Cardiology (JACC).
Metoprolol, a drug of the beta-blocker family, has been available for more than 30 years to treat arterial hypertension and other cardiovascular conditions.
In this new study, the team of researchers were able to examine the potential usefulness of metoprolol after a heart attack. The clinical trial named METOCARD-CNIC is the first to test metoprolol therapy, in heart attack patients undergoing standard angioplasty treatment procedures.
A total of 270 patients with infarction were recruited since 2010 in four of Spain's regions including: Madrid, Galicia, León, and Cantabria. In the randomized study, patients were assigned to receive either intravenous metoprolol or a placebo treatment at the moment of diagnosis of a myocardial infarction during ambulance transit to the catheterization laboratory.
Hospitals in Spain participating in the METOCARD-CNIC trial included: Hospital Clínico San Carlos, Hospital de La Princesa, Hospital 12 de Octubre, Hospital Puerta de Hierro, and Hospital Quirón (Madrid), Hospital Meixoeiro (Galicia), Hospital de León (León), and Hospital Marqués de Valdecilla (Cantabria).
The efficacy of the medical intervention was evaluated by magnetic resonance imaging (MRI) a week after the infarction. MRI measured the mass of damaged heart tissue in all patients. The results showed patients who received metoprolol had much smaller infarcts than those who received the control treatment, and that this smaller infarct size was linked to greater heart contractility.
The MRI scans were analyzed at the central CNIC laboratory by cardiologists blinded to the treatment.
Their preclinical research findings about metoprolol in animal models, analyzed using MRI and published in the journal Circulation in 2007, showed early administration of metoprolol during heart attack increased myocardial salvage.
The molecular mechanism leading to the beneficial effects is not clearly understood. It may have additional route of action, apart from decreasing the heart rate, myocardial contactability and decreasing the oxygen consumption; such as action on platelets and inflammation.
Metoprolol treatment is to be started in a patient, once the clinical parameters like bradycardia (Lower than normal heart rate) and hypotension (Lower than normal Blood pressure) are stabilized and the hemodynamic status had been carefully evaluated for signs of shock and congestive heart failure. Subjects are ineligible for treatment with metoprolol, if hypotension, bradycardia and peripheral shock are present.
Metoprolol to be started in haemodynamically stable patients with the intravenous administration of three bolus injections of 5 mg each at approximately 2 minutes of intervals. During the intravenous administration blood pressure, heart rate, and electrocardiogram are to be monitored.
In patients who tolerate the full intravenous dose (15 mg), Metoprolol tartrate is to be started orally, 50 mg every 6 hours; 15 minutes after the last intravenous dose and be continued for 48 hours. Thereafter, the maintenance dosage is 100 mg twice daily, at least for 3 months; and may be continued for 1 to 3 years according to some researchers.
Patients who appear not to tolerate the full intravenous dose, Metoprolol tartrate tablets may be started, either 25 mg or 50 mg every 6 hours (depending on the degree of intolerance) 15 minutes after the last intravenous dose or as soon as their clinical condition allows. In patients with severe intolerance, Metoprolol tartrate is to be discontinued.
In country like India, metoprolol treatment of myocardial infarction will be beneficial to many, even in the long term considering the cost of follow up treatment of the disease and its' complications; such as heart failure and arrhythmia.
...
Click here to Subscribe news feed from "Clinicianonnet; so that you do not miss out anything that can be valuable to you !!
...