You should not get swayed by your mammogram report that does not mention anything about the density of breast parenchyma, in spite of all normal findings.
According to legislation passed in Connecticut, the radiologist is expected to mention about the density of breast tissue. “Dense parenchyma” that “lowers the sensitivity of mammography”.
where applicable, such report shall include the following notice:
"If your mammogram demonstrates that you have dense breast tissue, which could hide small abnormalities, you might benefit from supplementary screening tests, which can include a breast ultrasound screening or a breast MRI examination, or both, depending on your individual risk factors. A report of your mammography results, which contains information about your breast density, has been sent to your physician's office and you should contact your physician if you have any questions or concerns about this report."
The Legislation can be viewed here.
This legislation was passed because of Nancy Cappello, a 61-year-old Connecticut woman. Her breast cancer had spread to her lymph nodes by the time it was diagnosed, even though she had had normal mammograms every year.
Ms. Cappello, the woman who started the movement to inform patients, began having yearly mammograms at age 40. In 2004, when she was 51, her doctor felt a lump in her breast, only six weeks after a mammogram had looked normal. Even after the lump was detected, mammography still could not find it. Only then, Ms. Cappello was told that she had dense breast tissue. The cancer had already spread to 13 lymph nodes. She needed a mastectomy, chemotherapy, radiation and hormone treatment.
Mammograms are scored on a five-point scale, using the following American College of Radiology Breast Imaging Reporting and Data System (BI-RADS) categories:
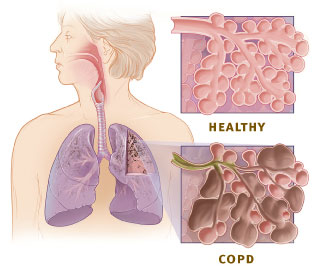
“Dense” breasts have a relatively high proportion of glandular or connective tissue, which blocks X-rays used in mammography. Non-dense breasts have more fat through which X-rays penetrate easily.
Over all, about 40percent of women who have mammograms have dense breast tissue. It is not abnormal, just one of nature’s variations. Younger women are more likely to have dense tissue, but as many as 25 percent of older women have it. Density cannot be judged by touch; it shows up only on mammograms.
In dense breast tissue, there is chance that abnormality may remain unnoticed. Something like, trying to see ice through ground glass. However,mammogram is gold standard, should not be ignored.
If it is a dense parenchyma, there is option for ultrasonogram (USG) and magnetic resonance imaging (MRI). USG and MRI are more sensitive than mammogram, but problem is that more often those give false positive results. False positivity may lead to unnecessary anxiety in patient and warrant more interventions like biopsy.
However, those are useful tool in case of dense breast parenchyma and indicated in case, there exist the risk factors for breast cancer, like strong family history and BRCA 1 or 2 mutation etc..
MRI may be used in women for evaluating;
That is why your radiologist must mention about density of breast parenchyma, if not, you should ask for it.
| Breast implant: Mammographs: Normal breast (left) and cancerous breast (right). (Photo credit: Wikipedia) |
According to legislation passed in Connecticut, the radiologist is expected to mention about the density of breast tissue. “Dense parenchyma” that “lowers the sensitivity of mammography”.
where applicable, such report shall include the following notice:
"If your mammogram demonstrates that you have dense breast tissue, which could hide small abnormalities, you might benefit from supplementary screening tests, which can include a breast ultrasound screening or a breast MRI examination, or both, depending on your individual risk factors. A report of your mammography results, which contains information about your breast density, has been sent to your physician's office and you should contact your physician if you have any questions or concerns about this report."
The Legislation can be viewed here.
This legislation was passed because of Nancy Cappello, a 61-year-old Connecticut woman. Her breast cancer had spread to her lymph nodes by the time it was diagnosed, even though she had had normal mammograms every year.
Ms. Cappello, the woman who started the movement to inform patients, began having yearly mammograms at age 40. In 2004, when she was 51, her doctor felt a lump in her breast, only six weeks after a mammogram had looked normal. Even after the lump was detected, mammography still could not find it. Only then, Ms. Cappello was told that she had dense breast tissue. The cancer had already spread to 13 lymph nodes. She needed a mastectomy, chemotherapy, radiation and hormone treatment.
Mammograms are scored on a five-point scale, using the following American College of Radiology Breast Imaging Reporting and Data System (BI-RADS) categories:
- Negative;
- Benign finding;
- Probably benign finding, short follow-up interval suggested;
- Suspicious abnormality, biopsy should be considered; and
- Highly suggestive of malignancy.
“Dense” breasts have a relatively high proportion of glandular or connective tissue, which blocks X-rays used in mammography. Non-dense breasts have more fat through which X-rays penetrate easily.
Over all, about 40percent of women who have mammograms have dense breast tissue. It is not abnormal, just one of nature’s variations. Younger women are more likely to have dense tissue, but as many as 25 percent of older women have it. Density cannot be judged by touch; it shows up only on mammograms.
In dense breast tissue, there is chance that abnormality may remain unnoticed. Something like, trying to see ice through ground glass. However,mammogram is gold standard, should not be ignored.
If it is a dense parenchyma, there is option for ultrasonogram (USG) and magnetic resonance imaging (MRI). USG and MRI are more sensitive than mammogram, but problem is that more often those give false positive results. False positivity may lead to unnecessary anxiety in patient and warrant more interventions like biopsy.
However, those are useful tool in case of dense breast parenchyma and indicated in case, there exist the risk factors for breast cancer, like strong family history and BRCA 1 or 2 mutation etc..
MRI may be used in women for evaluating;
- The integrity of silicone breast implants,
- Assessing cancers associated with silicon breast implant
- Assessing palpable masses following surgery or radiation therapy,
- Assessing for occult breast cancer in patients with axillary nodal metastasis found in mammogram or USG,
- Preoperative planning for some patients with known breast cancer.
- It has been promoted as a screening test for breast cancer among women at elevated risk of breast cancer based on BRCA1/2 mutation carriers, a strong family history of breast cancer, or several genetic syndromes such as Li-Fraumeni or Cowden disease.
That is why your radiologist must mention about density of breast parenchyma, if not, you should ask for it.
...
Click here to Subscribe news feed from "Clinicianonnet; so that you do not miss out anything that can be valuable to you !!
...